What Are The Latest Trends In Healthcare?
Are you curious about the latest trends in healthcare? Are you looking for ways to stay up-to-date on the newest innovations and developments in the healthcare industry? If so, then this is for you. We’ll explore some of the most exciting changes happening in healthcare today and what they mean for you.
In today’s rapidly evolving world, the healthcare industry is constantly adapting and incorporating new technologies to improve patient care and outcomes. Staying updated on the latest trends in education on healthcare is crucial for healthcare organizations to remain competitive and provide the best possible care to their patients. This blog will explore some of the key trends in healthcare that are shaping the industry in 2023.
Overview of the Healthcare Industry
The healthcare industry encompasses a wide range of sectors, including hospitals, clinics, pharmaceutical companies, medical device manufacturers, and more. The industry is driven by advancements in medical science, technology, and innovations in healthcare delivery models. With the growing aging population, increasing prevalence of chronic diseases, and the impact of the COVID-19 pandemic, the healthcare industry is under constant pressure to adapt and find new ways to meet the demands of patients and improve healthcare outcomes.
Importance of staying updated on healthcare trends
Staying updated on healthcare trends is essential for healthcare organizations to remain competitive and provide the best possible care to their patients. By staying informed about the latest innovations and technologies, healthcare organizations can:
- Improve patient outcomes: By adopting new technologies and treatment methods, healthcare organizations can provide more effective and personalized care to their patients.
- Enhance operational efficiency: New technologies can streamline administrative tasks, improve communication between healthcare providers, and enhance overall operational efficiency.
- Increase patient satisfaction: By offering innovative solutions and personalized care, healthcare organizations can improve patient satisfaction and loyalty.
- Stay ahead of competition: In a rapidly evolving market, staying up-to-date on healthcare trends is essential for healthcare organizations to remain competitive and attract new patients and talent.
By keeping an eye on the latest trends in healthcare, organizations can position themselves as leaders in the industry and drive positive change in patient care and outcomes.
In the next section, we will explore some of the key trends that are shaping the healthcare industry in 2023.
Artificial Intelligence in Healthcare
Artificial Intelligence (AI) has emerged as a game-changer in the healthcare industry, revolutionizing the way we diagnose and treat diseases. With the complexity and rise of data in healthcare, AI offers immense potential to improve healthcare outcomes. Here are some of the latest trends in AI application within healthcare:
Role of AI in improving healthcare outcomes
- AI has the ability to analyze vast amounts of medical data and identify patterns and insights that can help healthcare professionals make more accurate diagnoses and treatment recommendations.
- AI-powered virtual assistants and chatbots can provide personalized patient support, improve patient engagement, and enhance adherence to treatment plans.
- AI can automate administrative tasks, such as appointment scheduling and billing, freeing up healthcare professionals to focus more on patient care.
Applications of AI in diagnostics and treatment
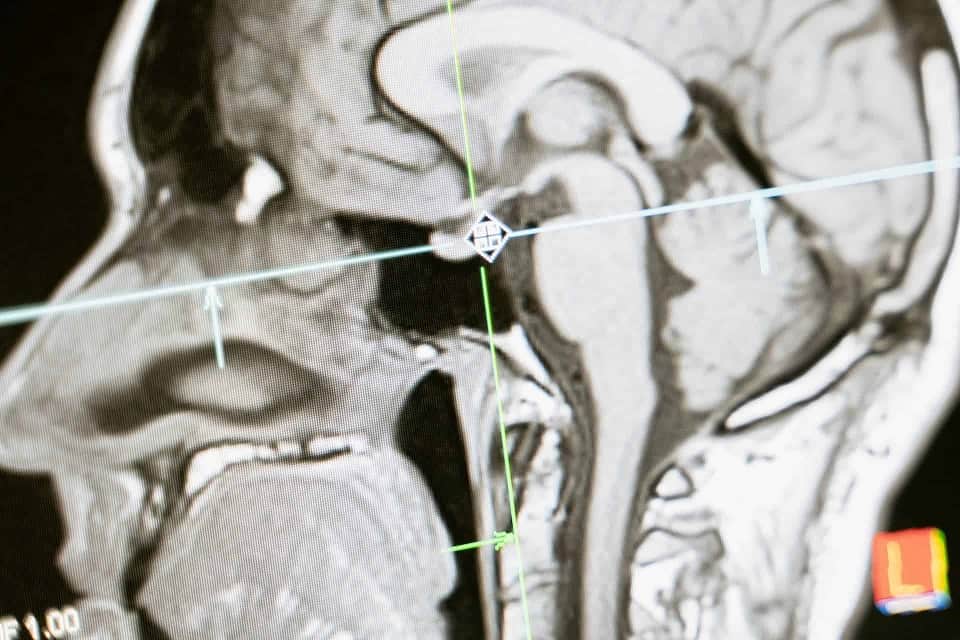
- AI algorithms can analyze medical images, such as X-rays and CT scans, to detect abnormalities and assist radiologists in making more accurate diagnoses.
- AI can predict disease progression and response to different treatment options, enabling healthcare professionals to develop personalized treatment plans.
- AI-powered robotic systems can assist surgeons during complex procedures, enhancing precision and reducing the risk of complications.
These advancements in AI have the potential to significantly improve patient outcomes, increase efficiency in healthcare delivery, and reduce healthcare costs. As AI continues to evolve, we can expect even greater innovations in the field of healthcare.

Personalized Healthcare
Understanding the concept of personalized medicine
Personalized healthcare, also known as precision medicine or personalized medicine, is a revolutionary approach to healthcare that takes into account the unique characteristics of each individual when it comes to prevention, diagnosis, and treatment of diseases. It recognizes that each person is different and that a one-size-fits-all approach may not be effective in providing optimal care.
In personalized medicine, healthcare providers use advanced technologies and data analysis to tailor medical decisions and treatments to the specific needs of each patient. This includes considering genetic, environmental, and lifestyle factors to develop targeted treatment plans. By understanding a person’s unique genetic makeup and other key factors, healthcare providers can deliver more precise and effective care.
Benefits of personalized healthcare for patients
Personalized healthcare offers several benefits for patients, including:
- Improved Accuracy: By considering individual characteristics, personalized healthcare enables more accurate diagnosis and targeted treatment plans for patients. This can lead to better health outcomes and reduced risks of adverse reactions or side effects.
- Enhanced Disease Prevention: Personalized medicine focuses on proactive measures to prevent diseases by identifying individual risk factors. Healthcare providers can develop personalized preventive strategies that help patients reduce their risk and take appropriate actions.
- Optimal Treatment Selection: Personalized medicine allows healthcare providers to choose the most effective treatment options for each patient based on their specific genetic and biological makeup. This can increase treatment success rates and reduce the need for trial and error.
- Increased Patient Engagement: Personalized healthcare empowers patients to actively participate in their own health management. By understanding their unique risks and treatment options, patients can make informed decisions about their healthcare and take the necessary steps to improve their well-being.
- Cost Savings: Personalized healthcare can potentially reduce healthcare costs in the long run by optimizing treatment plans, reducing the risk of unnecessary procedures, and improving health outcomes. It focuses on preventing diseases and providing targeted interventions, which can lead to more efficient resource utilization.
Overall, personalized healthcare represents a shift from a reactive approach to a proactive and individualized approach to healthcare. With advancements in technology and data analysis, personalized medicine has the potential to revolutionize the healthcare industry and improve patient outcomes.

Wearable Devices and Remote Monitoring
The use of wearable technology has seen a significant increase in recent years as consumers become more interested in monitoring their own health and wellness. This trend has also extended to the healthcare industry, where wearable devices and remote monitoring have played a crucial role in patient care. Here are some of the latest trends in wearable technology and remote monitoring:
The rise of wearable technology in healthcare
Wearable devices such as fitness trackers, smartwatches, and health monitors have become increasingly popular among consumers. These devices can track various health metrics such as heart rate, sleep patterns, activity levels, and even blood pressure. They provide users with real-time data that can help them stay informed about their health status and make informed decisions about their lifestyle.
Smart medical devices are another form of wearable technology that is gaining traction in the healthcare industry. These devices are designed to monitor specific health conditions and provide personalized care. For example, there are wearable devices available that can monitor glucose levels in diabetic patients, alerting them to any potential fluctuations or emergencies.
Remote monitoring and its impact on patient care
Remote monitoring allows healthcare providers to monitor patients’ health outside of traditional clinical settings. This is especially valuable for patients with chronic conditions who require continuous care and monitoring. Remote monitoring can be done through wearable devices that collect and transmit data to healthcare professionals, who can then analyze the data and provide appropriate interventions.
Some of the key benefits of remote monitoring include:
- Improved patient engagement in their own healthcare
- Enhanced adherence to treatment plans
- Increased access to care, particularly for patients who are unable to travel for in-person visits
- Reduced hospital readmission rates and emergency department visits
Here’s a comparison table to help you understand the different types of wearable devices and their features:
| Device Type | Features |
|---|---|
| Fitness Trackers | Heart rate monitoring, step counting, sleep tracking |
| Smartwatches | Health monitoring, GPS tracking, smartphone integration |
| Health Monitors | Blood pressure monitoring, glucose monitoring, ECG recording |
Overall, wearable technology and remote monitoring have revolutionized the healthcare industry by empowering patients to take control of their health and enabling healthcare providers to deliver more personalized and proactive care. As the technology continues to advance, we can expect to see even more innovative wearable devices and remote monitoring solutions in the future.

Telemedicine and Virtual Healthcare
The healthcare industry has witnessed a significant shift towards telemedicine and virtual healthcare in recent years. With advancements in technology and the need for accessible and convenient healthcare services, telehealth has become increasingly popular. Here are some of the latest trends in telemedicine and virtual healthcare:
The increasing popularity of telehealth services
- The COVID-19 pandemic has accelerated the adoption of telehealth services, as it has provided a safe and convenient way for patients to receive medical care without leaving their homes.
- Telehealth allows patients to consult with healthcare professionals remotely through video calls, phone calls, or online messaging.
- It provides access to medical care for individuals in remote or underserved areas, eliminating the need for extensive travel.
- Telemedicine has proven to be effective for routine check-ups, follow-up appointments, mental health consultations, and even primary care services.
Advantages and challenges of virtual healthcare
- Virtual healthcare offers several advantages, including:
- Convenience: Patients can schedule appointments and receive medical care from the comfort of their own homes.
- Cost savings: Telehealth services can reduce healthcare costs by eliminating the need for travel, parking, and other associated expenses.
- Improved access: Telemedicine allows patients to connect with healthcare professionals who may be located in different regions or countries, expanding access to specialized care.
- Better outcomes: Research has shown that virtual healthcare can lead to improved patient outcomes and satisfaction.
- However, there are also challenges to consider:
- Technological barriers: Not all individuals have access to the necessary technology or reliable internet connections, limiting their ability to participate in virtual healthcare.
- Privacy and security concerns: The transmission of personal health information over digital platforms raises concerns about patient privacy and data security.
- Limitations of virtual exams: Some medical conditions may require in-person examinations or diagnostic tests, which cannot be fully replicated through virtual healthcare.
Telemedicine and virtual healthcare have become integral parts of the healthcare industry, providing patients with convenient access to medical care. As technology continues to advance and healthcare providers adapt to this new mode of service delivery, telemedicine is likely to become even more prevalent in the future.

Social Determinants of Health
In the field of healthcare, there is growing recognition of the significant impact that social determinants of health have on individual and population health outcomes. Social determinants of health refer to the social and economic factors that shape the conditions in which people are born, grow, live, work, and age. These factors include income, education, employment, housing, and access to healthcare. Understanding and addressing social determinants of health is crucial for achieving health equity and providing patient-centered care.
Exploring the impact of non-medical factors on health outcomes
Research has consistently shown that individuals who experience poverty, limited education, and social disadvantage are more likely to face health problems and have shorter lifespans. Even in affluent countries like ours, disparities in health outcomes persist based on socioeconomic status. These disparities are deeply rooted in systemic issues such as structural racism, inequality, and lack of access to resources.
It is important for healthcare professionals to recognize the influence of social determinants on health outcomes and take action to address them. By understanding the social context in which patients live and work, clinicians can provide more holistic and patient-centered care.
Efforts to address disparities in healthcare access and outcomes
Addressing social determinants of health requires a multi-faceted approach. Healthcare professionals can play a crucial role in advocating for policy changes, conducting research, and implementing interventions to address the social factors that affect health.
Some concrete actions that healthcare professionals can take to address social determinants of health include:
- Asking patients about their social history, including questions about housing, employment, education, and social support.
- Providing patients with information and resources related to social services, such as food assistance programs, housing support, and job training.
- Referring patients to community organizations that address social determinants, such as community health centers, social workers, and community outreach programs.
- Collaborating with other healthcare professionals, community organizations, and policymakers to advocate for changes in social policies that improve health outcomes.
It is important for healthcare professionals to be aware of the social determinants of health and incorporate them into their practice. By addressing these factors, we can work towards reducing health disparities and promoting health equity for all individuals and communities.

Behavioral Medicine
The connection between mental and physical health
In recent years, there has been a growing recognition of the strong connection between mental and physical health. It is now well-established that mental health disorders can increase the risk of developing chronic physical conditions, such as diabetes, heart disease, and respiratory conditions. Conversely, individuals with chronic physical conditions are more likely to experience mental health disorders like anxiety and depression. This bidirectional relationship highlights the importance of addressing both mental and physical health in order to improve overall well-being and quality of life.
Innovative approaches to behavioral medicine
To meet the growing demand for integrated care, innovative approaches to behavioral medicine are emerging. These approaches aim to provide comprehensive care that addresses both mental and physical health needs. Some of the latest trends in behavioral medicine include:
- Telehealth and digital interventions: The use of telehealth and digital interventions has seen significant growth, particularly during the COVID-19 pandemic. These technologies enable individuals to access mental health services and support remotely, making care more accessible and convenient.
- Data-driven interventions: Advances in data analytics and artificial intelligence allow for personalized and data-driven interventions in behavioral medicine. By analyzing large datasets, healthcare providers can identify patterns and tailor interventions to individual needs, improving treatment outcomes.
- Collaborative care models: Collaborative care models bring together primary care providers, mental health specialists, and other healthcare professionals to provide coordinated care. These models aim to seamlessly integrate mental health services into primary care settings, ensuring that both mental and physical health needs are addressed.
- Behavioral health integration in specialty settings: Integrating behavioral health services into specialty settings, such as oncology or cardiology clinics, allows for a more holistic approach to care. By addressing the psychological impact of a specific condition, healthcare providers can better support patients throughout their treatment journey.
- Digital therapeutics: Digital therapeutics, such as smartphone applications and wearable devices, offer evidence-based interventions for mental health conditions. These interventions can help individuals monitor their symptoms, learn coping skills, and track progress, providing support outside of traditional therapy sessions.
Overall, the latest trends in behavioral medicine emphasize the importance of integrating mental and physical health care. By addressing the connection between mental and physical health, healthcare providers can offer more comprehensive and effective care to improve patient outcomes.

Retail Healthcare
In recent years, we have witnessed a significant shift in the healthcare industry with the rise of retail healthcare. This trend involves the integration of healthcare services into retail settings such as pharmacies, big-box stores, and shopping malls. Retail healthcare offers a convenient and accessible option for individuals to access medical care. Let’s take a closer look at the benefits and implications of this emerging trend.
Benefits of Retail Healthcare:
- Convenience: Retail healthcare locations offer extended hours, same-day appointments, and walk-in services, making it easier for individuals to receive the care they need without having to take time off from work or school.
- Cost-Effectiveness: Retail healthcare locations are often more affordable than traditional healthcare settings, providing an accessible option for individuals with limited budgets.
- Quality of Care: Many retail healthcare locations are staffed by qualified healthcare professionals, such as nurse practitioners and physician assistants, who can diagnose and treat minor illnesses. These locations are equipped with state-of-the-art medical equipment to provide advanced treatments.
Implications of Retail Healthcare:
- Disruption of the Healthcare Landscape: With their consumer-centric focus, deep pockets, and widespread reach, retailers are well-positioned to compete with traditional health systems and physician practices in the healthcare space.
- Expansion of Services: Retail clinics have evolved from providing basic non-emergency care to offering more advanced primary care, chronic disease management, and even behavioral health services.
- Changing Patient Behavior: The convenience and transparent pricing offered by retail healthcare providers align with the consumer’s desire for more accessible and affordable care, potentially shifting patient behavior away from traditional healthcare settings.
Retail healthcare is transforming the way individuals access and experience medical care. The integration of healthcare services into retail settings offers convenience, cost-effectiveness, and quality of care. As this trend continues to expand, it will be interesting to observe how it shapes the future of healthcare delivery.

Unbundled Healthcare and Alternative Insurance Options
With the changing landscape of healthcare, new trends are emerging that are reshaping the industry. Two trends that have gained traction in recent years are the rise of alternative insurance models and unbundled healthcare services.
The rise of alternative insurance models
Traditional health insurance plans have limitations and may not always meet the needs of individuals and families. This has led to the emergence of alternative insurance options that offer more flexibility and customization. Some of the popular alternative insurance models include:
- Health Savings Accounts (HSAs): An HSA is a tax-advantaged savings account that allows individuals to save money for medical expenses. It is paired with a high-deductible health plan (HDHP) and offers tax benefits.
- Direct Primary Care (DPC): DPC is a membership-based model where patients pay a monthly fee to access comprehensive primary care services. This model eliminates the need for insurance claims for routine visits and allows for more direct access to healthcare providers.
- Health Sharing Ministries: Health sharing ministries are organizations where members pool their resources to cover healthcare costs. Members contribute a monthly amount, and the funds are used to pay for eligible medical expenses.
Unbundled healthcare services and their impact on affordability
Unbundled healthcare services refer to the ability to choose specific services or procedures instead of purchasing a comprehensive insurance plan that covers everything. This allows individuals to pay only for the services they need, potentially reducing costs. Some examples of unbundled healthcare services include:
- Telemedicine: Telemedicine allows patients to connect with healthcare providers remotely, eliminating the need for in-person visits for minor ailments. This not only saves time but also reduces healthcare costs.
- Cash-Based Services: Some healthcare providers offer cash-based services, where patients pay directly for services without involving insurance companies. This can be an affordable option for routine services or minor procedures.
- Medical Tourism: Medical tourism involves traveling to another country to receive medical treatments at a lower cost. It has gained popularity as a way to access quality healthcare at a fraction of the cost compared to some countries.
The latest trends in healthcare are focused on providing more options and affordability for individuals and families. Alternative insurance models and unbundled healthcare services are giving consumers more control and flexibility over their healthcare decisions, potentially reducing costs and increasing access to care. These trends are likely to continue shaping the healthcare industry in the future.
Recapping The Latest Trends In Healthcare
Keeping up with the latest trends in healthcare is crucial for both healthcare professionals and patients. These trends are shaping the future of healthcare and have the potential to greatly improve patient outcomes and experiences. Here are some key takeaways from the latest trends in healthcare:
Staying up to date with the latest trends in healthcare is essential for healthcare professionals to deliver high-quality care and for patients to make informed decisions about their health. Embracing these trends can lead to better patient outcomes, improved access to care, and increased efficiency.



